Hybrid Claims Data: The Essential Strategy for Enhanced RWE and HEOR Studies
In the pursuit of robust Real-World Evidence (RWE) and impactful Outcomes Research (HEOR), one element stands out above all else: data completeness. While traditional single-source datasets, such as “closed-only claims” from individual commercial payers, have been the norm for years, they inevitably leave gaps. These blind spots hinder a full understanding of a patient’s healthcare journey, which in turn limits the strength and accuracy of research findings and the ability to draw meaningful conclusions. This perspective is further explored in our recent article featured on The Evidence Base, where Forian experts discuss how hybrid claims data is transforming RWE and HEOR research.
At Forian, we contend that the current limitations and gaps in healthcare data are unacceptable. Our proposed solution is hybrid claims data, which involves the strategic integration of closed claims (single-payer data) with comprehensive open claims (multi-source, aggregated data). This methodology enables researchers to move beyond incomplete records and achieve a more comprehensive, patient-focused understanding of healthcare utilization.
.png?width=500&height=500&name=Hybrid%20Claims%20Data%20Blog%20Image%201%20(3).png)
Figure 1. Closed claims represent only the visible portion of healthcare costs, while open claims reveal the hidden layers of patient care and utilization.
The hybrid approach offers clear advantages:
- Maximized cohorts: larger and more representative patient populations that strengthen statistical power.
- Total economic picture: captures all care, including critical carve-outs such as specialty drugs and behavioral health.
- Richer clinical detail: overlapping records are merged to provide a clearer, more nuanced view of patient encounters.
- Extended follow-up: overcomes patient turnover to deliver critical longitudinality.
The industry increasingly acknowledges the value of this data linkage. Extensive research at major HEOR conferences and in peer-reviewed literature highlights the necessity of robust, multi-source data to mitigate bias and improve analytical precision. Hybrid claims data is transitioning from an advantage to an essential component.
.png?width=310&height=217&name=ISPOR%20Blog%20Image%201%20(1).png)
Below, we break down four critical ways hybrid claims data enhances RWE and HEOR studies, transforming data limitations into actionable insights.
1. Maximizing Study Populations and Generalizability with Hybrid Claims
Hybrid data offers a significant advantage in scaling research by overcoming the limitations of traditional closed claims data. Closed claims inherently restrict study populations to individuals with continuous enrollment under a single payer, resulting in smaller cohorts and reduced statistical power. This limitation is particularly impactful for studies focusing on rare diseases or specific sub-populations.
By utilizing open claims, hybrid claims data enables the creation of continuous patient activity metrics that mirror closed enrollment data. This broader perspective allows researchers to mitigate selection bias and include a larger number of patients who meet study criteria, even if their coverage history is non-contiguous or mixed. The inclusion of these additional patients, who would otherwise be excluded due to enrollment gaps, leads to a more representative and generalizable cohort, thereby minimizing common selection biases inherent in single-payer analyses.
The benefit of a larger, more inclusive cohort extends to bolstering statistical power. With an increased volume of patient data, researchers can uncover meaningful patterns, identify treatment effects with greater precision, and draw conclusions supported by stronger evidence. These enhanced insights are vital as they have the potential to influence clinical guidelines, inform regulatory decisions, and guide payer coverage policies.
2. Capturing Carve-Outs and the True Total Economic Burden
Hybrid data offers a crucial corrective lens, revealing the true economic and clinical burden of a condition that primary insurance alone often fails to capture, even when a patient is actively enrolled in a commercial closed claims plan.
By integrating open claims data with closed claims, researchers can gain visibility into critical care encounters, often termed "carve-outs," which are paid outside the primary commercial plan. Specific examples include:
- Alternate coverage: claims paid by Medicare, self-pay arrangements, or supplemental commercial insurance, which are often crucial for understanding the patient journey as they age or shift employment.
- Eliminating pharmaceutical data gaps: closed claims often contain significant limitations in visibility into pharmacy benefit drug utilization, particularly for specialty products, or they may entirely "carve-out" specific therapeutic areas, such as complex behavioral or mental health services. Hybrid claims ensure accurate tracking of every prescription dispensed and every high-cost specialty infusion administered, providing a complete picture of therapeutic adherence and total resource utilization.
Combining these factors provides a more precise representation of the patient journey and the actual cost of care. By considering all carve-outs, researchers can more accurately quantify the economic burden of disease, which is crucial for informing policy, enhancing access, and guiding decisions.
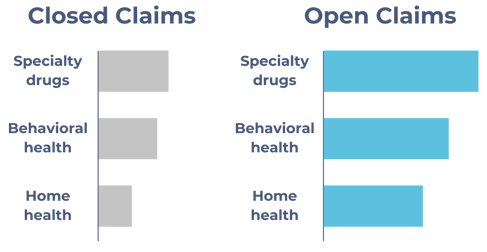 Figure 2. Traditional closed claims significantly underrepresent costs for critical categories like specialty drugs and behavioral health. Integrating open claims exposes these "carve-outs," providing a complete and accurate view of total utilization.
Figure 2. Traditional closed claims significantly underrepresent costs for critical categories like specialty drugs and behavioral health. Integrating open claims exposes these "carve-outs," providing a complete and accurate view of total utilization.
3. Enhancing Encounter Detail for Deeper Clinical Context
Hybrid data doesn't just mean more claims; it also makes existing records better. Often, both open and closed claims feeds will mention the same doctor visits or hospital stays. By bringing these overlapping records together, you get a much fuller and more detailed picture of what happened. This means researchers can dig up extra clinical, procedural, and diagnostic info for the same patient visit.
For example, one source might give you the main diagnosis and procedure codes, but if you merge in a second source, you could get details like who referred the patient, secondary diagnoses, or other services tied to that event. This combined view turns what would be a pretty basic claim into a much richer, more useful piece of data.
This extra level of detail is important for accurate "phenotyping," which helps us be more precise when looking at things like co-occurring conditions, how well interventions work, and defining patient groups. Plus, it leads to more reliable RWE and HEOR modeling because it cuts down on the guesswork from claims that aren't fully coded or are incomplete.
4. Expanding Longitudinality to Minimize Patient Turnover
Reliance on commercial closed claims data presents a significant limitation due to the abrupt loss to follow-up when patients switch payers or employment. The inherent volatility of commercial enrollment severely compromises long-term outcomes studies, leading to a substantial portion of patients being annually lost to follow-up. This creates a critical challenge for studies requiring extended observation periods, such as research into long-term safety or chronic disease progression.
Hybrid data addresses this challenge by offering continuous patient tracking across disparate payers and data feeds. This ensures that crucial outcomes, including cost, safety events, and subsequent treatments, are captured over a meaningful timeframe, thereby enhancing the robustness of RWE/HEOR studies.
Conclusion and Next Steps
For RWE and HEOR studies to truly reflect the complex, multi-payer reality of the U.S. healthcare system, researchers must move beyond the confines of closed claims. Hybrid claims data offers a strategic path forward, delivering the increased sample size, complete data capture, detailed encounters, and crucial longitudinality needed to generate statistically sound and market-ready evidence.
To learn more about how Forian is solving the longitudinality challenge and minimizing patient attrition, we invite you to read our external article featured on The Evidence Base.
Coming Soon: Over the next few months, we will dive deeper into the remaining 3 specific use cases through dedicated blog posts. Each will feature data-driven case studies that demonstrate how hybrid claims data expands patient cohorts, captures the true cost of care, and optimizes encounter detail. These deep dives will highlight the practical impact of a more complete data foundation and how it can drive better research, stronger evidence, and smarter decision-making. Stay tuned!



.jpg?width=50&name=Image%20from%20iOS%20(2).jpg)
